
Pressure sores, also known as pressure ulcers or bedsores, are injuries to the skin and deeper tissues caused by prolonged pressure. They often affect individuals who are bedridden, use wheelchairs, or have limited mobility. Without proper care, these wounds can lead to severe complications. This guide offers practical steps for caregivers and healthcare professionals to prevent, identify, and treat pressure sores effectively.

Understanding the Causes of Pressure Sores
Pressure sores occur when blood flow is restricted due to sustained pressure on the skin, especially over bony areas like the tailbone, hips, heels, and elbows. This deprives tissues of oxygen and nutrients, leading to skin breakdown and tissue damage.
Contributing Risk Factors:
- Shear and friction during movement or repositioning
- Moisture exposure from sweat or incontinence
- Chronic conditions such as diabetes, poor circulation, or malnutrition
People with reduced mobility or sensation are at the greatest risk. Caregivers need to be proactive about identifying early warning signs to prevent complications. Pressure sores occur when blood flow is restricted due to sustained pressure on the skin, especially over bony areas like the tailbone, hips, heels, and elbows. This deprives tissues of oxygen and nutrients, leading to skin breakdown and tissue damage.
Contributing Risk Factors:
- Shear and friction during movement or repositioning
- Moisture exposure from sweat or incontinence
- Chronic conditions such as diabetes, poor circulation, or malnutrition
People with reduced mobility or sensation are at the greatest risk. Caregivers need to be proactive about identifying early warning signs to prevent complications.
Classification of Pressure Sores
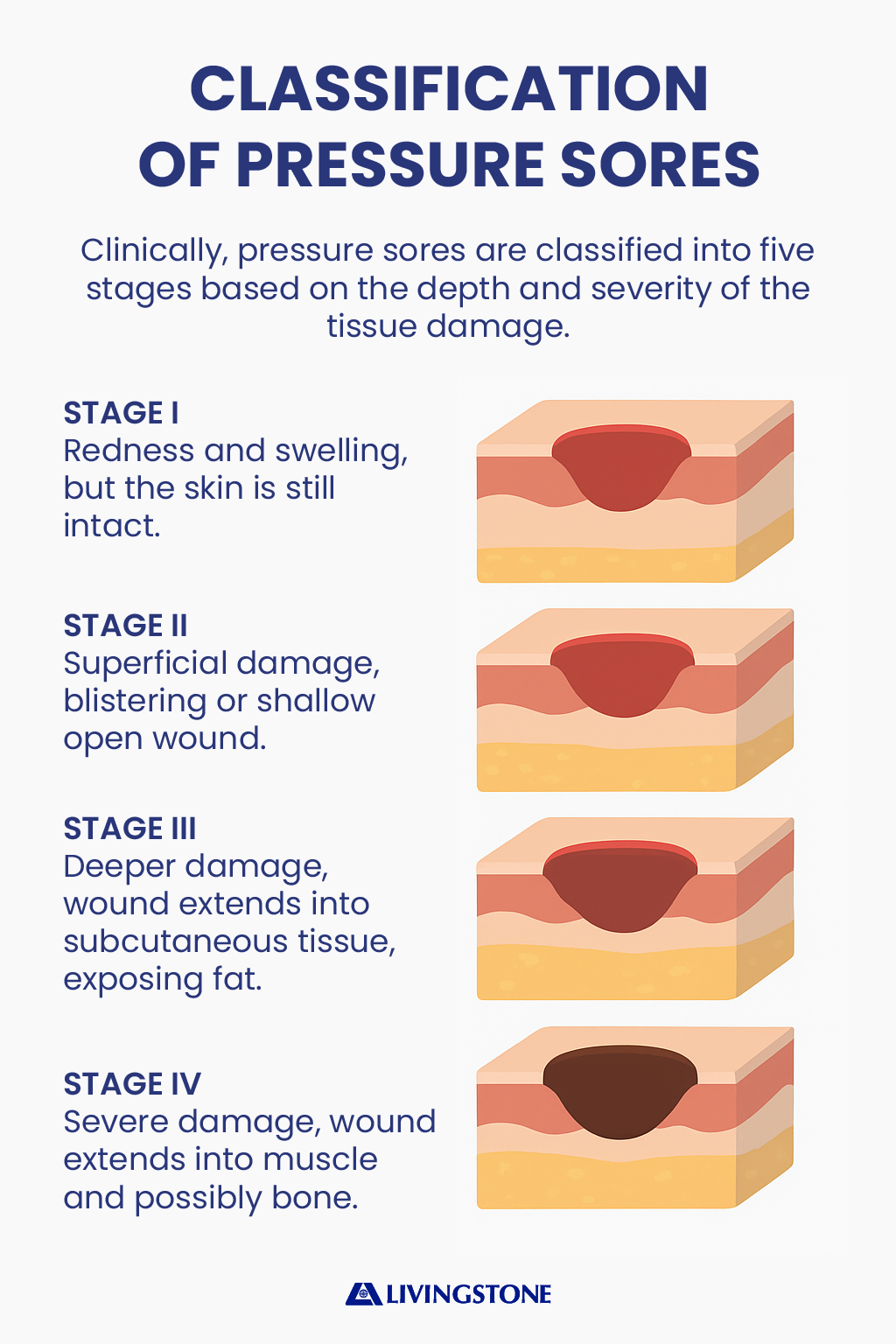
Clinically, pressure sores are classified into five stages based on the depth and severity of the tissue damage. In Stage I, the skin remains intact but appears red and does not blanch when pressed. Stage II involves superficial damage with blistering or shallow open wounds. In Stage III, deeper layers of skin and subcutaneous tissue are affected, exposing fat. Stage IV presents the most severe damage, extending into muscles and possibly bone. An unstageable sore is one where necrotic tissue covers the wound, obscuring its true depth until debridement is performed.
Effective Treatment Strategies for Pressure Sores
Proper wound care is essential to recovery. Treating pressure sores involves a mix of relieving pressure, cleaning wounds, and supporting healing from within.
Relieve Pressure First
- Reposition patients at least every two hours when lying down
- Encourage weight shifts every 15 minutes when seated
- Use pressure-relieving cushions and mattresses to reduce strain on vulnerable areas
Clean and Dress the Wound
- Use saline or gentle cleansers to clean the area
- Apply appropriate dressings based on the wound’s condition:
- Hydrocolloid dressings for shallow wounds
- Foam dressings for moderate drainage
- Alginate dressings for wounds with heavy exudate
Remove Dead Tissue When Necessary
If the wound contains slough or necrotic tissue, debridement is needed. This can be done through:
- Surgical removal
- Autolytic debridement (using moisture-retentive dressings)
- Enzymatic methods
Watch for Infection and Act Quickly
Infected pressure sores need immediate attention. Warning signs include:
- Redness and warmth around the wound
- Swelling or pus
- Foul odour
- Fever or chills
Treatment may require topical antiseptics or systemic antibiotics, depending on severity. Never ignore signs of infection, especially in higher-stage ulcers.
Managing Chronic and Non-Healing Wounds
For sores that persist despite standard care, more advanced interventions may be required. Negative Pressure Wound Therapy (NPWT) can aid healing by drawing out fluid, reducing swelling, and promoting tissue growth. In severe cases, surgical repair using flap techniques might be considered. Emerging therapies such as hyperbaric oxygen therapy or electrical stimulation can further enhance healing by increasing oxygenation or encouraging cellular regeneration.
The Role of Nursing Care Plans
Nurses are central to both the prevention and management of pressure sores. Comprehensive care plans begin with risk assessments using validated tools. Setting measurable goals—like reducing wound size or preventing new sores—is essential. Regular documentation of interventions, changes in wound status, and patient response enables informed adjustments to the care plan.
Patient and family education is also critical. Teaching proper skin inspection, positioning techniques, and nutritional guidance empowers carers and promotes adherence to treatment strategies.
Practical Tips for Prevention and Daily Care
Preventing pressure sores requires diligence and a proactive mindset. Reposition patients frequently and use moisture barriers to protect skin from incontinence. Skin should be inspected daily, focusing on bony prominences and areas exposed to friction. Maintaining hydration and a balanced diet not only promotes overall health but also enhances skin resilience. Caregivers should tailor interventions to the patient’s unique needs and consistently communicate with the care team. Most importantly, educating both patients and caregivers fosters a team approach to prevention
Pressure sores are a preventable and treatable condition when addressed with informed care practices. Understanding their causes, recognising early warning signs, and implementing evidence-based interventions can lead to positive outcomes. Through collaboration, education, and ongoing monitoring, caregivers and clinicians can significantly improve the quality of life for those at risk.
References
Australian Wound Management Association (2022). Pan Pacific Clinical Practice Guideline for the Prevention and Management of Pressure Injury. Available at: https://www.awma.com.au/publications/ (Accessed: 24 April 2025).
Better Health Channel (2023). Pressure sores. Victorian Government. Available at: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/pressure-sores (Accessed: 24 April 2025).
Wound Australia (2023). Wound management resources and standards. Available at: https://www.woundaustralia.com.au (Accessed: 24 April 2025)
