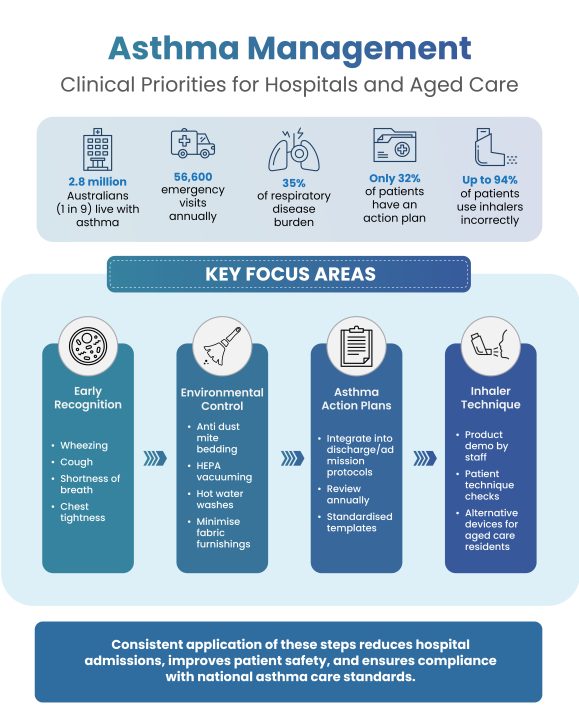
Asthma Awareness Week 2025 highlights the critical need for hospitals, aged care providers, and healthcare facilities to strengthen respiratory management protocols and reduce preventable admissions. With 2.8 million Australians living with asthma, representing 11% of the population, the condition continues to impose a significant burden on both patients and the healthcare system.
Asthma is the leading cause of disease burden in children aged 1–9 years, disrupting early development and increasing paediatric hospitalisation rates. Across all age groups, asthma contributes to 35% of the total respiratory disease burden, with 56,600 annual emergency department presentations recorded nationwide. For healthcare leaders, these figures reinforce the importance of evidence-based strategies that reduce reliance on acute care and improve long-term outcomes.
Early Recognition and Clinical Intervention
Early identification of asthma flare-ups remains a core responsibility for hospital and aged care staff. Symptoms such as wheezing, persistent coughing, shortness of breath, and chest tightness should prompt immediate clinical review.
In acute settings, delayed recognition increases the likelihood of emergency escalation, prolonged admissions, and additional strain on already stretched respiratory services. Within aged care facilities, where residents often present with multiple comorbidities, staff must be trained to recognise subtle changes in breathing patterns and escalate appropriately. Embedding structured observation and escalation protocols ensures consistency of care across teams.
Managing Dust Mite Allergen Exposure in Facilities
Environmental triggers are a significant driver of uncontrolled asthma. Dust mite allergens, in particular, are one of the most common exacerbating factors in Australian healthcare and residential settings. These allergens accumulate in bedding, upholstered furniture, and carpets, making facilities high-risk environments if not managed correctly.
Facilities can reduce exposure through:
- Procurement of dust mite–proof bedding covers for wards and residential rooms.
- Implementing laundering protocols that include hot water washes above 60°C for sheets and pillowcases.
- Regular HEPA-filter vacuuming in patient areas to capture fine allergens.
- Limiting heavy curtains and fabric furnishings in high-risk rooms.
These measures not only improve outcomes for patients with asthma but also demonstrate compliance with best practice environmental controls. Resources for allergen management and patient support are available from the National Asthma Council Australia.
Integrating Asthma Action Plans into Patient Management
Despite decades of advocacy, only 32% of Australians with asthma have a written asthma action plan. This is a critical gap in care. Action plans outline the steps a patient and their carers should take when symptoms escalate, providing a clear framework for managing exacerbations and avoiding unnecessary hospitalisation.
In hospital discharge planning and aged care admission protocols, the inclusion of an asthma action plan should be a standard requirement. Plans support continuity of care across multiple providers and ensure that both staff and families are confident in responding to an acute episode.
Action plans must be reviewed annually and adjusted for age, comorbidities, and medication regimens. Standardised templates and clinical guidance are outlined in the Australian Asthma Handbook, which sets the national standard for asthma care.
Improving Inhaler Technique in Clinical Practice
Data indicates that up to 94% of patients do not use their inhaler devices correctly. This remains one of the most significant barriers to effective asthma control. Incorrect technique results in suboptimal drug delivery and increases the risk of uncontrolled symptoms, emergency visits, and repeat admissions.
Hospitals and aged care facilities must embed inhaler technique assessments into routine practice. Nurses, pharmacists, and allied health professionals should regularly demonstrate correct usage and confirm patient capability, particularly during discharge planning or medication reviews. For residents with dexterity limitations or cognitive decline, alternative delivery devices should be considered.
By standardising these checks, facilities can directly reduce preventable exacerbations and improve medication adherence.
Addressing Poor Asthma Control in Younger Populations
Asthma control issues are not limited to older adults or paediatric patients. Twenty-seven percent of Australians under 40 have poor asthma control based on their medication use. This group is particularly prone to underusing preventer inhalers, relying heavily on relievers, and underestimating the risks of unmanaged symptoms.
Hospitals and clinics play an essential role in reinforcing adherence during emergency presentations, while aged care staff supporting younger residents must also monitor medication use closely. Consistent messaging across healthcare providers is essential to shift patterns of poor control and reduce the burden on acute services.
Strengthening Asthma Care in Healthcare Facilities
Asthma Awareness Week 2025 underscores the importance of structured respiratory care across hospitals, aged care services, and healthcare facilities. With millions of Australians affected and tens of thousands of preventable hospital visits each year, consistent application of evidence-based guidelines is critical.
By integrating asthma action plans into patient management, monitoring inhaler technique, addressing allergen control, and embedding ongoing staff training, healthcare organisations can significantly improve patient outcomes while reducing system-wide pressures.
For hospitals, aged care providers, and procurement teams, prioritising asthma management is both a clinical responsibility and an operational imperative.
References
- National Asthma Council Australia (2025) National Asthma Council Australia. Available at: https://www.nationalasthma.org.au (Accessed: 1 September 2025).
- National Asthma Council Australia (2025) Australian Asthma Handbook. Available at: https://www.asthmahandbook.org.au (Accessed: 1 September 2025).
