Nebulisers play a vital role in managing respiratory conditions by delivering medication directly into the lungs. For patients living with asthma, chronic obstructive pulmonary disease (COPD), or other breathing difficulties, these devices offer an effective method of treatment that can be easily managed at home or in clinical settings. Understanding how nebulisers work, their role in asthma care, and how they compare to inhalers is essential for healthcare professionals, caregivers, and patients alike.
How do nebulisers work?
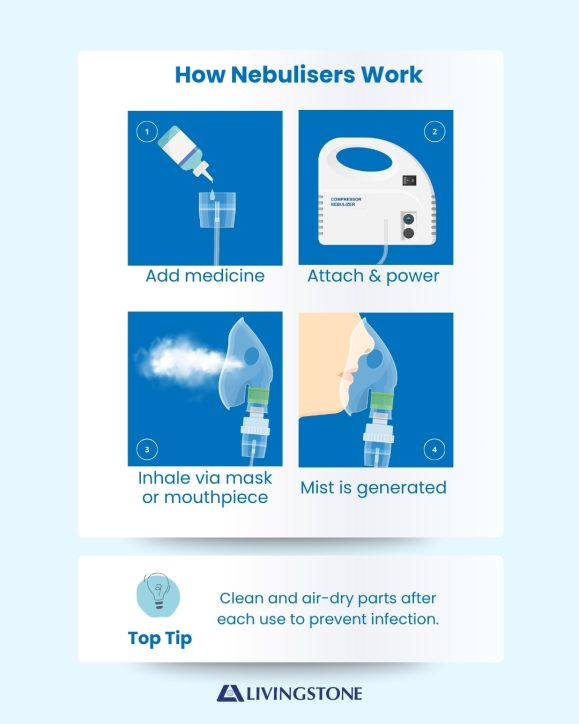
A nebuliser is a medical device that converts liquid medication into a fine mist that can be inhaled through a mask or mouthpiece. Unlike inhalers, which rely on the patient’s ability to coordinate breathing with actuation, nebulisers provide a continuous flow of medication during normal breathing. This makes them particularly helpful for young children, elderly patients, or those experiencing severe respiratory distress.
Nebulisers typically operate using one of three methods:
- Jet nebulisers: The most common type, which uses compressed air to break medication into aerosol particles.
- Ultrasonic nebulisers: Use high-frequency vibrations to generate a mist, producing faster delivery and quieter operation.
- Mesh nebulisers: Incorporate a vibrating mesh to push medication through fine holes, creating consistent and portable treatment.
This targeted delivery ensures medication reaches the lower airways, allowing for faster symptom relief and improved absorption where it is needed most.
Is it safe to use a nebuliser with asthma medications?
Nebulisers are commonly prescribed to administer bronchodilators and corticosteroids for patients with asthma. When used as directed by a healthcare professional, they are safe and highly effective. Nebulised therapy can be particularly beneficial during acute asthma attacks when patients struggle to coordinate inhaler use or when larger doses of medication are required.
According to Asthma Australia, nebulisers are suitable for specific situations but are not always the first-line treatment. While they provide reliable medication delivery, healthcare providers typically recommend inhalers with spacers for daily management, reserving nebulisers for severe flare-ups or hospital-based care.
Patients using nebulisers at home should follow strict hygiene practices to minimise infection risks. This includes cleaning and disinfecting the mouthpiece, mask, and medication chamber after each use. Regular replacement of tubing and filters is also important to ensure consistent performance.
What equipment is needed for home respiratory care?
For individuals managing chronic respiratory conditions at home, having the right equipment ensures both safety and comfort. A basic home respiratory care kit may include:

- Nebuliser machine: Portable or tabletop, depending on patient needs.
- Mask and mouthpiece sets: Sized appropriately for adults or children.
- Tubing and medication chamber: Essential components that must be cleaned and replaced regularly.
- Spacer device: For those also using metered dose inhalers.
- Peak flow meter: To monitor lung function and detect early signs of deterioration.
- Pulse oximeter: A non-invasive tool to check blood oxygen saturation.
Families and caregivers should also have clear guidance from healthcare providers on how to prepare medication, maintain equipment, and respond to worsening symptoms. The National Asthma Council Australia offers helpful fact sheets and device guidelines to support safe use at home.
Are nebulisers better than inhalers for asthma patients?
Whether a nebuliser is better than an inhaler depends on the individual’s condition, preferences, and level of symptom control. Inhalers, particularly when used with spacers, are generally preferred for long-term asthma management because they are portable, fast-acting, and cost-effective. They also deliver medication with less wastage compared to some nebuliser models.
Nebulisers, however, remain an important tool for certain groups of patients. Children under the age of five, elderly individuals with reduced coordination, and patients experiencing severe asthma attacks often benefit more from nebulised treatment. In emergency settings, nebulisers allow healthcare providers to administer continuous high-dose medication efficiently, which can be life-saving during acute episodes.
It is also worth noting that advances in technology have made modern nebulisers more compact, quieter, and easier to use. Mesh nebulisers, in particular, combine portability with precision, bridging the gap between traditional inhalers and large tabletop devices.
Ultimately, the choice between nebulisers and inhalers should be guided by a healthcare professional, who will consider factors such as disease severity, lifestyle, and frequency of symptoms. Many patients use both devices at different times, with inhalers for day-to-day control and nebulisers reserved for more severe episodes.
Supporting better respiratory outcomes
Nebulisers continue to play a significant role in respiratory care, providing reliable relief for those who struggle with traditional inhalers. While not a replacement for prescribed daily treatments, they are a valuable tool for managing acute episodes and ensuring medication delivery in vulnerable patient groups.
For healthcare providers, ensuring patients understand how to use and maintain their nebulisers is as important as prescribing the right medication. Proper education on cleaning, replacing parts, and monitoring symptoms empowers patients to take charge of their respiratory health and improves long-term outcomes.
As technology evolves, nebulisers are becoming more efficient, user-friendly, and accessible. When combined with a comprehensive asthma management plan, they remain a cornerstone of care for patients across Australia.
References
- Asthma Australia. (2023). Asthma medications and devices. Available at: https://asthma.org.au/about-asthma/asthma-management/medication/ (Accessed: 29 September 2025).
- National Asthma Council Australia. (2023). Nebulisers factsheet. Available at: https://www.nationalasthma.org.au/living-with-asthma/resources/patients-carers/factsheets/nebulisers (Accessed: 29 September 2025).
- Global Initiative for Asthma (GINA). (2024). GINA Report, Global Strategy for Asthma Management and Prevention. Available at: https://ginasthma.org/gina-reports/ (Accessed: 29 September 2025).
- Australian Institute of Health and Welfare (AIHW). (2022). Asthma. Available at: https://www.aihw.gov.au/reports/chronic-respiratory-conditions/asthma (Accessed: 29 September 2025).